When CIM Director David Hellmann describes the research mission of Johns Hopkins rheumatologist Max Konig, he uses an analogy drawn from the movies — Clint Eastwood’s Dirty Harry character, who sets out to clean up a corrupt San Francisco police department by taking out the handful of “bad cops” who are ruining the entire system.
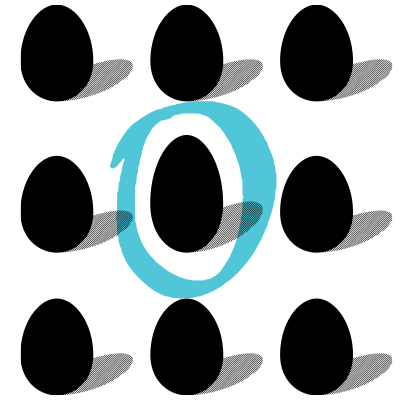
“Our immune system is like the police system of our body, and when we encounter autoimmune diseases, it’s due to a few ‘bad cops’ attacking the normal citizens in our body,” says Hellmann. “Just as Clint Eastwood selectively goes after each of the bad cops, leaving the good cops in place to protect us, so Dr. Max Konig is working to develop precision therapies that will leave the ‘good cops’ unharmed, allowing patients to escape the complications that are so common with current therapies for autoimmune disease.”
Konig, an assistant professor who completed his residency training at Harvard and advanced training in rheumatology at Johns Hopkins before joining the faculty, is now at the leading edge of a promising new line of investigation. He is capitalizing on cellular therapy approaches that have become the standard of care in treating cancer to develop precision treatments for devastating autoimmune diseases like lupus, rheumatoid arthritis and antiphospholipid syndrome, which is implicated in heart disease, stroke and pregnancy loss.
“Although we are at the very edge of the journey,” says Konig, “there is a sense of enormous potential to use engineered cell therapies to create tailored solutions to prevent, control and cure autoimmune diseases.”
He is motivated by a sense of urgency, since existing treatments for autoimmune diseases carry potentially toxic side effects that can be debilitating and even deadly. That’s because only a tiny percentage of cells drive autoimmune disease, “but as rheumatologists, we currently have to use an armamentarium of drugs to ‘burn down the whole forest’ to get control of that very small population,” he explains. The impact on patients of this toxicity? A high risk of infection, poor response to vaccines and treatment-related deaths.
“Although we are at the very edge of the journey, there is a sense of enormous potential to use engineered cell therapies to create tailored solutions to prevent, control and cure autoimmune diseases.” – Max Konig
Konig is building on advances in CAR T-cell therapy, a type of immunotherapy that is increasingly being used to treat patients with B cell-driven blood cancers, including lymphoma, leukemia and multiple myeloma. Simply explained, the treatment involves collecting a patient’s “killer” T cells, then reengineering those cells to recognize and attack the cancer by binding to proteins, or antigens, on the cancer cells’ surface. Different types of cancer have different antigens, so each type of CAR T-cell therapy is made to fight a specific kind of cancer antigen.
After being reengineered, the cells are allowed to multiply and then infused back into the patient to do their cancer-fighting work.
“It’s remarkable that this works — that CAR T cells can actually cure blood cancers,” says Konig. “This is no simple feat. In order to cure a cancer, you need to get rid of every single last cell or the cancer will come back.”
The success of CAR T treatment has led Konig and others to wonder: “If we have such a unique and incredibly powerful tool to cure B cell cancers, could it be applied to treat B cell-driven autoimmune diseases?” He and others believe the answer is “yes.”
“We are on the verge of the next step in treating autoimmune diseases, one that will bring us into a new era of cell engineering and cellular therapies,” says Konig, “where all of a sudden we have the tools to design really tailored solutions.”
He points to early clinical trials in Germany in five young adults with moderate to severe lupus who had not responded to existing treatments. After undergoing B cell-targeted CAR T treatment (which eliminates good and bad B cells alike), “all these patients were in complete clinical and immunological disease remission,” he says. Other researchers have taken a similar strategy and produced similarly encouraging remission outcomes in patients with MS spectrum disease and myositis.
In his lab at Johns Hopkins, Konig and his colleagues in the Ludwig Center, part of the Kimmel Cancer Center, are furthering this strategy by developing and using a new generation of T cell therapy approaches — such as CRISPR-based engineering of chimeric autoantigen-T cell receptors — to reprogram a patient’s T cells so they can selectively target self-reactive immune cells while safeguarding normal immune populations.
“These precision therapies have the potential to transform the lives of patients living with autoimmune and rheumatic diseases by providing new tailored treatments that can control autoimmunity without increasing the risk of infection that is common to all existing treatments,” Konig notes.
The “hope message” Konig is eager to share? “I really think engineered cellular therapies will enable a future where we can treat, prevent and cure autoimmune diseases.”