We all can attest to the fact that COVID-19 has been very hard on Hopkins caregivers as we witness human suffering, and we are all at increased risk of anxiety, stress, and mental exhaustion. What can we at Johns Hopkins do to care for each other and nurture each other’s resilience?
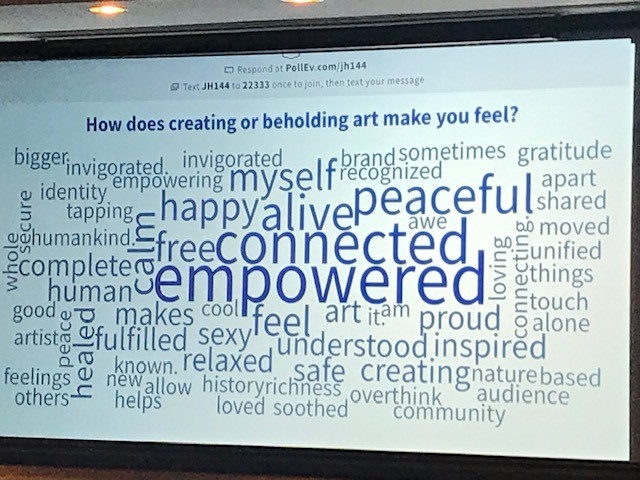
On December 1st, Susan Magsamen presented a CIM Seminar, “Caregivers and the Arts: Cultivating Joy, Gratitude & Renewal,” to discuss how we might explore caregiver arts experiences to fortify spirit, teamwork, and dignity.
Magsamen is the founder and director of the International Arts + Mind Lab (IAM Lab), the Center for Applied Neuroaesthetics from the Pedersen Brain Science Institute within Johns Hopkins University School of Medicine. IAM Lab’s work encompasses research, community building, and outreach and education centered on the intersection of brain sciences and the arts, and how our unique response to art can amplify human potential. Magsamen is an award-winning author of seven books as well as the Impact Thinking Model, a translational research approach to solving problems in learning, healing, and wellbeing through the arts. Additionally, Magsamen is the co-director of the NeuroArts Blueprint Initiative in partnership with The Aspen Institute.
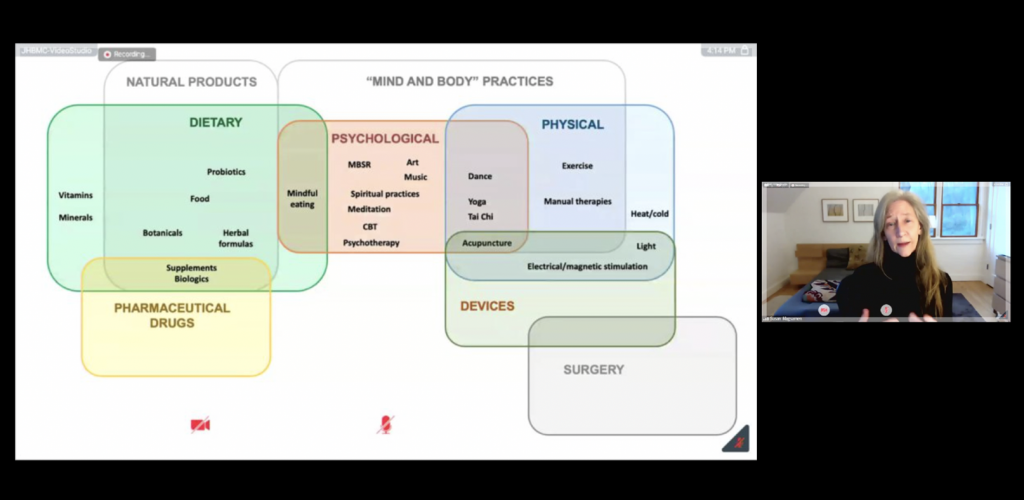
Here she is below discussing an interesting illustration developed by the National Institutes of Health, examining where the arts sit within clinical care; essentially, the arts bridge psychological and physical components of health and wellbeing. Consequently, it may have tremendous health benefits to proactively foster “Mind and Body” practices.
Magsamen seeks to leverage the IAM Lab’s resources in a structured, intentional way to energize and expand arts experiences within the Hopkins community. As a starting point, she recommends the establishment of an Arts, Health, and Wellbeing Working Group, expressly to facilitate innovative caregiver arts initiatives within the School of Medicine. The workgroup would: review proposals and provide technical assistance; award seed funding to initiatives; document programmatic outcomes; showcase successes; and develop a scalable model for replication and implementation elsewhere throughout the university. Magsamen’s concept to create an arts-based healing community with Hopkins gained favorable enthusiasm from CIM seminar participants, many of whom shared their personal stories about healing through music and other art forms. CIM cares about the wellbeing of Hopkins caregivers, and we endorse the concept of an IAM Lab Arts, Health, and Wellbeing Working Group to benefit our healing community.
Also, we reviewed some of the important resources currently available to caregivers within the Hopkins community through the Office of Well-Being; please visit them online to review the full array of help available:
As 2020–a year of unprecedented challenges in our lifetime–comes to an end, may you find peace, comfort and hope in 2021’s potential. Meanwhile, if you feel beleaguered, please ask for support, and consider the healing power of the arts to cultivate joy, gratitude, and renewal.
CIM sends best wishes for a safe, healthy holiday!
For further reading about healing power of the arts, see these articles in Neuron:
Each partner in the alliance for a Human Aging Project (HAP) has committed to funding faculty members who will collaborate on this bold initiative. The CIM, for example, announced funding for these new CIM HAP Scholars:

Dr. Peter Abadir is the Salisbury Family CIM HAP Scholar. Dr. Abadir is an Associate Professor of Medicine in the Division of Geriatric Medicine and Gerontology. His research interests include: changes in the Renin Angiotensin Aldosterone system with aging; signal transduction and the role of the cross talk between Angiotensin II receptor in aging; and understanding the role of angiotensin II in development of vascular aging. Dr. Abadir delivered a powerful presentation for the CIM in July, at which we announced the pan-university, interdisciplinary alliance among the Schools of Business, Engineering, Medicine, and Nursing to create an innovative HAP; a superb researcher, his past experiences collaborating with colleagues across the university serves as the model for our building our ambitious HAP’s organizational goals.
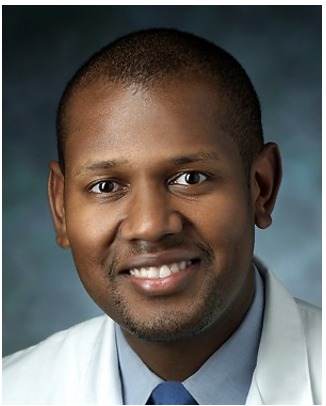
Dr. Thomas Cudjoe has been named the Caryl & George Bernstein CIM HAP Scholar. A 2020 recipient of the Junior Faculty Teaching Award, Dr. Cudjoe is an Associate Professor of Medicine in the Division of Geriatric Medicine and Gerontology. His recent research and publications have been about social isolation, financial and social determinants of health vis-à-vis aging in place, accessible housing and mobility concerns, and advanced care planning, among others. And those are just some of the reasons why he was named among the 125 Hopkins Heroes in 2018 as part of our 125th Anniversary. In addition to being a Hopkins Hero, Dr. Cudjoe has a strong reputation for infusing caring into his teaching and research, yielding meaningful health equity findings with impact.

Dr. Rasika Mathias received the Sarah Miller Coulson CIM HAP Scholar award. Her research lab focuses on the genetics of asthma in people of African ancestry, and led to the first genome-wide association study of its kind. Dr. Rasika Mathias is an Associate Professor of Medicine in the Division of Allergy and Clinical Immunology, and she maintains a joint appointment in the Division of General Internal Medicine at the Johns Hopkins School of Medicine as well as the Department of Epidemiology at the Johns Hopkins Bloomberg School of Public Health. Like Dr. Cudjoe, she brings a wealth of pioneering research findings that address healthcare inequities, bringing social justice to medicine.
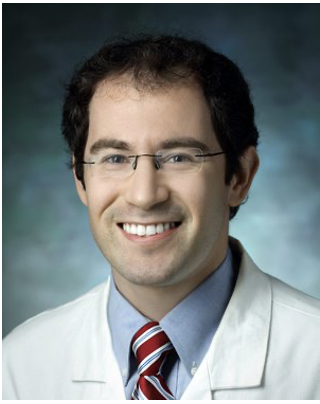
Dr. Alex Pantelyat was awarded the Alafouzos Family CIM HAP Scholarship. He is an Assistant Professor with Neurology, the Director of the Atypical Parkinsonism Center, a Co-Founder and Co-Director of the Johns Hopkins Center for Music & Medicine, and a Co-Director of the Johns Hopkins Movement Disorders Fellowship. His research explores: atypical Parkinsonian disorders (such as dementia with Lewy bodies, progressive supranuclear palsy, corticobasal syndrome/degeneration and multiple system atrophy); cognitive aspects of movement disorders; and music-based rehabilitation of neurodegenerative diseases. His innovative research is truly about the medical arts.
We are proud to sponsor these fabulous four physicians with CIM scholarships especially for advancing the HAP. Each CIM HAP Scholar has demonstrated a commitment to both the field of aging, and to Medicine as a Public Trust. We congratulate them for their accomplishments leading to this distinct honor, and we eagerly anticipate reporting on how their CIM HAP scholarships will enable them to extend as long as possible robust and healthy aging, and to minimize and postpone the disabilities that can occur as we age.
Read more about the HAP in our Winter 2020 edition of Breakthrough here.

Jessica Long, a decorated US Paralympian, will be the keynote speaker at the 5th annual Medicine for the Greater Good (MGG) Symposium—Celebrating 30 Years of the Americans With Disabilities Act—on Thursday, November 10th from Noon to 3 p.m. via Zoom as part of Johns Hopkins Bayview’s Department of Medicine Grand Rounds:
Zoom Link: https://jhjhm.zoom.us/j/94679924762?pwd=QUloYWRFaDJqVnZSVXJ5eGlDQy9idz09
Meeting ID: 946 7992 4762
Passcode: 315645
A global inspiration, Jessica Long is a World Champion Para-Swimmer and 13-time Paralympic Gold Medalist. With 23 Paralympic medals altogether, she is the second-most decorated Paralympian in US history. Long grew up in Baltimore, but she is originally from Siberia, where she was adopted from a Russian orphanage at 13 months old. Born with fibular hemimelia, she was missing the fibulas, ankles, heels, and most of the other bones in her feet. At 18 months old, her legs were amputated below the knees so she could be fitted for prosthetic legs and learn to walk. Long fell in love with swimming in her grandparents’ backyard pool. She joined her first competitive swim team at the age of 10. Just two years later, she competed in the Paralympic Games Athens 2004 as the youngest athlete on Team USA. Now 27 years old, she has collected 13 Paralympic gold medals, 31 world titles, and multiple world records. Long has inspired others to chase their dreams throughout her career, and she has found a new sense of purpose by giving back.

Following Long’s keynote speech, CIM Scholar and MGG co-founder and co-director Dr. Colleen Christmas, Director, Primary Care Leadership Track and Associate Professor of Medicine with the Division of Geriatric Medicine and Gerontology, will moderate a panel discussion on caring for patients with disabilities. Panelists include:
The US Department of Justice Civil Rights Division’s website about the Americans with Disabilities Act (ADA) states, “Throughout this 30th anniversary year, the Civil Rights Division is recognizing the many ways in which the ADA has transformed American society and enabled a generation of Americans with disabilities to thrive. At the same time, we recognize that many barriers to equal opportunity still remain. We recommit to our work of making the promise of the ADA a reality, enabling all Americans with disabilities to achieve their dreams and reach their full potential.” Dr. Christmas told CIM that she is “really excited about the focus of the MGG symposium in celebrating the 30th anniversary of the passing of the ADA. This was one of the most important pieces of civil rights legislation passed in our country codifying the rights of people with disabilities to have the same access to opportunities to fully participate in society as anyone else.”
Emceeing the event will be CIM Scholar and MGG co-founder and co-director Dr. Panagis Galiatsatos, Director of the Tobacco Treatment Clinic and Assistant Professor with Pulmonary and Critical Care Medicine, as well as co-chair of the Johns Hopkins Health Equity Steering Committee. “We are excited to celebrate the importance of the ADA’s 30th anniversary with Jessica in her home City of Baltimore, and we are excited to raise awareness on the ability for persons with disabilities to persevere,” added Dr. Galiatsatos.
“This is a cause worth celebrating, yet part of the purpose of the MGG symposium is to explore both the victories and where we continue to fall short in realizing that promise fully. It is exciting to consider the work ahead that will continue to move us towards the goal of equity for all and the excellence that emerges from diversity and inclusion,” said Dr. Christmas.
MGG is grateful to Jessica Long, Trevon Jenifer, Jessica Campanile, Harry Paul, and Drs. Tracy Friedlander and Bonnielin Swenor for participating in this event, and MGG thanks the event sponsors: the JH Office of Diversity, Inclusion & Health Equity; JHM Language Services; JHU Connects; Janssen; and the Pharmaceutical Companies of Johnson & Johnson.
For further information, contact Anne Kennan at akennan1@jhmi.edu or 410-550-9890.
Special Announcement for Center for Innovative Medicine International Advisory Board Members: The in-person annual IAB meeting previously scheduled for October 12th will now be held via Zoom. Dr. Hellmann will be contacting IAB members soon with details. Thanks for your understanding. Stay safe and well!
Dear Friends:
While we won’t be able to gather together for our 6th Annual Center for Innovative Medicine Retreat in August this year for obvious reasons, we do want you to know that the ideas convened at our past retreats are very much alive, robust and kicking!
Most significantly, last year’s retreat formally launched the start of the “Human Aging Project” (“HAP”) – a clarion call to look anew at the concept and idea of aging – aging well, aging better, partnering with science, clinical practice and technology, joining together with all of Johns Hopkins remarkable assets – its people and its many schools – to make aging a focus of our ingenuity and creativity.
Great ideas have a way of either falling by the wayside – they are too big or too audacious – or they have a way of gaining steam and becoming real. Thanks to all of you who have participated in the Center for Innovative Medicine retreats in the past, the ideas that were once flying around at last year’s retreat are now being implemented, and have become very real.
As an update, the “Human Aging Project”, led by Dr. Jeremy Walston, now has an internal advisory board and working group who convene regularly. It has committed partners, such as the Johns Hopkins Schools of Medicine, Engineering, Nursing, Public Health, the Carey School, and others. Its expanse reaches across many of JHU’s departments and divisions within and outside of medicine. We are pleased to let you know that the Center for Innovative Medicine will soon be able to fund a new class of CIM Scholars who will singularly focus on an aspect of aging as it relates to the Human Aging Project.
We will miss being together in person this year, but we are very much together in spirit, and look forward to being back at Folly Farm next year. Thank you for believing in the Center for Innovative Medicine and for being a major contributor to its life force and ideas.
Mark your calendars: CIM Retreat: Thursday, August 26, 2021, 8-2pm!
With kindest regards,
David B. Hellmann, M.D.; Aliki Perroti Professor of Medicine & Director, Center for Innovative Medicine
Stephanie Cooper Greenberg; Chair, International Advisory Board, Center for Innovative Medicine
On July 14th, CIM facilitated a very successful and productive collaborative presentation via Zoom with 180 stakeholder participants to launch a multidisciplinary Human Aging Project—including the Johns Hopkins Carey School of Business, the Whiting School of Engineering, the School of Medicine, and the School of Nursing—aimed at extending as long as possible robust and healthy aging, and at minimizing and postponing the disabilities that can occur as we age.
Translational scientist Dr. Peter Abadir, Associate Professor of Medicine in the Division of Geriatric Medicine and Gerontology, led the presentation about this exciting new health care alliance aimed at bringing together students and faculty from different disciplines to create innovation incubators at Johns Hopkins Bayview Medical Center to generate practical solutions to vexing problems in patient care for older adults today and tomorrow. During the 90-minute presentation, participants heard from key stakeholders:
After the group heard from the university leadership, several faculty and students from across the university described ways in which they have collaborated. Dr. Jeremy Walston, Raymond and anna Lublin Professor of Geriatric Medicine and the Deputy Director for the Division of Geriatric Medicine and Gerontology, has been leading the effort behind the Human Aging Project. Dr. Walston shared examples of past collaborations between Engineering and Medicine focusing on Apple products and blood pressure regulation. And Dr. Walston stated an initial clear goal: To bring all of these pan-university resources together and push bioengineering, aging, and many clinical programs related to the emergency room or surgical safety program. Over time, the goal is to become a global epicenter to further develop the interactions with students and faculty to collaborate and generate innovations to improve the health and wellbeing of older adults.
Dr. Yousef Yazdi, Director of the Johns Hopkins Center for Bioengineering Innovation and Design, piggybacked on Dr. Walston’s remarks. Dr. Yazdi highlighted that elder care is still a huge underserved market, and that his center was created around 11 years ago around existing science and tech to solve real world problems. “Success demands attention to organizational strategy,” he added, emphasizing three aspirations for the Human Aging Project innovation incubators; that they: focus on clinical needs; have commercial potential; and have tech end-design in mind for the user. These guiding principles have led his center to 84 projects, $40M in startup equity, and clinical mentors from 26 departments, including a fellowship program for medical students and partnerships across JH and the industry. Their design teams have an interest in addressing needs in aging, and his center is eager to deploy the resources to improve the lives of the elderly.
Following Dr. Yazdi’s presentation, the group heard from students from business and engineering who have already engaged in healthcare-related projects with resounding success. For instance, Kevin Keenahan of Tissue Analytics, Inc., created 3D wound-imaging software to create a smartphone app that can measure and diagnose wound tissues, and the data can be easily integrated into EPIC. Dr. Alissa Murphy, who runs the Multidisciplinary Design Course, spoke of how important user-centered design is in the innovative process, and several student teams described their successes with innovations benefiting Blind Industries Services Maryland, as well as a biomedical engineering project to reduce catheter-related urinary tract infections, known as Urineflo.
Having illustrated by examples how interdisciplinary collaborations have already proven effective at Johns Hopkins among several stakeholders that serendipitously involve aging issues, Dr. Peter Abadir presented a detailed outline to start with 5 incubators (consisting of 2-3 engineering students, 2 business students, and two doctors or nurses) specifically designed to encourage breakthroughs in geriatric care. The incubators would have two phases: discovery; and accelerator mode. They would focus on themes, such as telehealth, remote sensing, robotics devices, human factors, big data, therapeutics, life space and social engagement, and wearable and implantable devices.
To conclude, Dr. Walston explained where CIM is in the process and next steps. Having served as a source of startups and incubators for 16 years, CIM will continue to sponsor any initiatives, and Human Aging Project funding would be funneled through CIM. He and CIM are asking for funding throughout the university.
Finally, Dr. David Hellman expressed gratitude to Drs. Mark Anderson and Cynthia Boyd, who have also expressed support for the Human Aging Project. And Dr. Hellmann thanked the students on the call whose success at similar projects are inspiring. Clearly, with superb structure and adequate funding, the Human Aging Project will be able to bring medicine together with other partners to advance the field and address some of the health consequences of aging. Dr. Hellman stated that this is the spearhead of the effort, and there would be follow up with call participants in small groups and as individuals to gather feedback. The plan is to start recruiting student participants this Fall.
And, in summation, Dr. Hellmann quoted Halford E. Luccock, “No one can whistle a symphony. It takes a whole orchestra to play it.” To that point, CIM thanks the leadership from Business, Engineering, Medicine, and Nursing for their strong support, and we especially appreciate the student presentations, as well as Dr. Peter Abadir for so clearly conceptualizing the practical logistics to implement the innovation incubators within the Human Aging Project, and Dr. Jeremy Walston for championing the subject over the years at CIM Annual Retreats.
On Tuesday, May 12th, Dr. Hellmann gave the 17th Annual Miller Lecture entitled “Bayview: Johns Hopkins’ Ode to Joy” to a remote audience with greater than 160 viewers. (Due to COVID-19 safety precautions, the 17th Annual Miller Lecture was held via Zoom only.) This reflection is only a quick overview of tone and the main themes covered in Dr. Hellmann’s speech. Johns Hopkins community members with a JHED ID may log in to experience a video recording of the lecture here.
Johns Hopkins Bayview Medical Center’s Board of Trustees Chair Charlie Scheeler introduced Dr. Hellmann as a “Renaissance Man”–a gifted scientist, physician, and a story-teller. His genius was evident in this fabulous lecture, which Dr. Hellmann dedicated to the “curious, smart, and well-read” Anne Miller. Throughout the lecture, Dr. Hellmann thanked the Miller Family and key leaders throughout Johns Hopkins for their steadfast support, sharing the conviction that are at the core of Bayview’s success: Medicine as a Public Trust.
“Bayview: Johns Hopkins’ Ode to Joy” underscored that Medicine as a Public Trust is Johns Hopkins’ North Star principle, demonstrated how the Johns Hopkins Bayview Medical Center has flourished under that guiding star, and asserted that Bayview is Johns Hopkins’ “Ode to Joy” as a result of intentionally and unwaveringly following Medicine as a Public Trust. And Dr. Hellmann expressed that sentiment through a brilliant musical metaphor to Beethoven’s 9th Symphony.
As you may know, Dr. Hellmann translates Johns Hopkins’ tripartite mission as triple-stranded DNA: the primordial strand of Caring, the essential basis of good medicine; the innovative strand of Science, furthering medicine; and the strand of Justice related to health, pursuing health equity. He asserts that Hopkins’ triple-stranded DNA is what makes us different, that those components are critical to Making Medicine a Better Public Trust, and that we must never lose sight of pursing those aspects of medicine.
For each of the three essential musical instruments to the melody in the 4th Movement of Beethoven’s 9thSymphony (“Ode to Joy”), he identified a Johns Hopkins community member who is not only a physician, but who is also a musician: Dr. Matthias Holdhoff (cello of caring); Dr. Bela Turk (viola of science); and Dr. Nestoras Mathioudakis (violin of justice related to health). As the “Medicine as Public Trust” Trio, they played together/apart, and gave a performance worthy of a standing ovation at Baltimore’s Hippodrome Theater. During the solo and ensemble performances, Dr. Hellmann encouraged the audience to reflect on Caring, Science, and Justice in health—and how powerful they are together in delivering the promise of medicine and making medicine a better public trust.
There has been significant growth and marvelous change at Johns Hopkins Bayview Medical Center over the last 20 years. Coincidentally, this is the same span of time that Dr. Hellmann has served as Chairman of Bayview’s Department of Medicine. Since he arrived at Bayview, he has collaborated with many outstanding leaders, transforming Bayview into an internationally respected part of the Johns Hopkins system. Throughout the lecture, Dr. Hellmann provided specific examples of precision medicine, transformative education in supporting the MERIT Leadership Academy, to name only a few. Dr. Hellmann pointed to numerous examples in education innovation, research capacity and collaboration, recognized national rankings for several medical divisions, a revenue-producer for Johns Hopkins Department of Medicine’s bottom line, and more. And Dr. Hellmann expressed gratitude for the many people who supported his efforts throughout the years.
Certainly, Dr. Hellmann is a maestro at story-telling, and this was a very personal, heart-felt story for him to tell. In a sense, this lecture is a symphony of ideas and accomplishments, paying tribute to his beloved Bayview and to those who made it what it is today. His affection for the Miller Family—especially Anne—rang clear and true. And this speech was personal and moving for Dr. Hellmann for yet another reason; in July, Dr. Hellmann will step down as Chair of the Department of Medicine and as Vice Dean of the School of Medicine at Bayview. Dr. Hellmann’s Miller Lecture was, in a way, his “swan song” and a love letter to Bayview and some of its greatest supporters, collaborators, and partners in making medicine a better public trust.
After the Medicine as a Public Trust Trio performed Beethoven’s sweet “Ode to Joy,” the piece took on new personal meanings, probably as Dr. Hellmann intended. Now, it is as if that music rejoices in Bayview and in the Miller Family as its wise benefactors.
For many of us viewing the lecture, and unbeknownst to Dr. Hellmann—a man with a great heart who brings meaning to everything he touches—this Ode to Joy now also warmly reflects our profound admiration for him, and you can hear a chorus of viewers expressing their gratitude to Dr. Hellmann at the end of the video.
Listen to the 17th Annual Miller Lecture here, and feel the joy! (Johns Hopkins credentials are required to log in and view the Grand Rounds recording.)
The Miller Coulson Academy of Clinical Excellence recognizes those who epitomize making medicine a better public trust through exemplary clinical care. Unfortunately, facing the COVID-19 pandemic, the 12th Annual Miller Coulson Academy of Clinical Excellence Induction Ceremony, which was to have been held on March 27, 2020, was cancelled. Despite the lack of fanfare, these remarkable clinicians are absolutely worth celebrating. This year, the Academy received twenty applicants and almost 300 unique nominations. Among nominations, that is about a 40% increase from 2019. Also, in its deliberations, the Academy was even more selective than last year; they typically induct 10 members—for 2020, they selected only nine:
Additionally, 24 physicians received the Frank L. Coulson, Jr., Resident Award for Clinical Excellence, and 16 individuals received awards for their superlative roles as a Nurse Practitioner or Physician Assistant.
The CIM would like to congratulate all of these amazing members of the Johns Hopkins Medicine family. At times like these, it is important that we hold each other up in the light and recognize and cherish our good works —individually and as a team; each person honored by the MCACE in its 12th year is a role model.
Finally, the CIM would like to thank the Miller Coulson and Worley families for their gracious support to recognize these great clinicians.
Sadly, the JHBMC Doctor’s Day Breakfast celebration planned for Monday, March 30th was canceled in compliance of precautionary COVID-19 guidelines. Ironically during this chaotic and disheartening time, our physicians are most deserving of a celebration of appreciation. To all physicians and healthcare workers, please know that now more than ever, Johns Hopkins Bayview Medical Center is grateful for what you do!
At the breakfast, physicians would have received a symbolic token of appreciation; Wande Kotun, Director of Population Health, designed a beautiful print depicting red carnations, an international symbol for Doctor’s Day. As some of you may also know, Wande is a wonderful artist, and you may have seen her work unknowingly throughout Baltimore City, or read about her in the news, or heard her speak on a panel at Medicine for the Greater Good’s symposium last fall on Arts & Medicine. Here is an image of the artwork she created for physicians on their special day:
We are most grateful to report that the Roche Family Foundation has sponsored a Center for Innovative Medicine, and we are joyful to announce that Dr. Michael Fingerhood is the recipient!
For more than a quarter of century in his leadership role with the Comprehensive Care Practice at Bayview, Dr. Fingerhood has been pivotal to innovating patient-centered care—especially for those with substance use disorders. Here is a quote from Dr. Fingerhood’s Closler blog:
“I’ve devoted my career to a love of primary care and as a passionate advocate for patients with substance use disorders, through direct patient care, teaching, research and community activism. I lead the division of Chemical Dependence within the Department of Medicine at JHBMC, and also have a joint appointment in the Bloomberg School of Public Health. I was an inaugural member of the Miller Coulson Academy of Clinical Excellence and an early blogger for the Academy.”
Many thanks to the Roche Family Foundation for supporting Dr. Fingerhood with the distinct honor of a CIM Scholarship!
Among the many meetings and events affected by the global pandemic, those sponsored by the Center for Innovative Medicine (CIM) have also been affected. In particular, the bi-monthly CIM Seminars are suspended until at least May. Other large events that have been cancelled include:
For a complete list of cancellations, visit: https://www.hopkinsmedicine.org/coronavirus/cancellations.html
For more information on what our health system is doing about this health crisis, please visit the Johns Hopkins Coronavirus Resource Center: https://coronavirus.jhu.edu
As we publish this blog, CIM Scholar Brian Garibaldi, MD, is in the trenches fighting for those suffering with COVID-19 in his role as the Director of the Johns Hopkins Biocontainment Unit. It is the only one of its kind in the region. An interview with him will be the keystone article in our upcoming edition of Breakthrough. Meanwhile, here are a few recent stories about what he has been doing to prepare for this pandemic as it hits Baltimore.

At a recent CIM seminar, Francoise Marvel, MD, Cardiovascular Fellow at Johns Hopkins, gave a talk entitled, “A New Frontier of Innovative Digital Medicine and Healthcare Delivery,” which reveals a great model for collaboration and innovation to develop digital care solutions to some of today’s most challenging patient care issues.
Dr. Marvel has a clinical interest in digital health, precision medicine, developing innovative healthcare transformational technology and delivery systems that connect health with the human experience in a seamless way. She is Co-Founder of Corrie Health, a digital innovation framework aimed at transforming healthcare deliver, empowering patient self-management, and preventing avoidable 30-day hospital readmissions for heart attack patients.
Corrie Health is the result of collaborations within and external to Hopkins: Johns Hopkins Medicine; the Whiting School of Engineering; the Carey Business School; and the Apple accelerator. Together they have reinvented heart attack recovery. Corrie Health personalizes and empowers the heart attack recovery patient experience in the hospital and at home, and it can be made accessible for underserved survivors. To learn more about Corrie Health, and to watch an introduction to Corrie, visit: https://corriehealth.com/
Future directions for Corrie Health include iShare loaner iPhones, digital biomarkers and predicate analytics, and a virtual cardiac rehab. The possibilities and potential seem endless when it comes to transforming AMI, AFIB, and cardiovascular care that is highy-personalized precision medicine.
Dr. Marvel has been recognized for this breakthrough work by Johns Hopkins Linda Dunbar Award for population health and health system transformation, American College of Physicians, American College of Cardiology, American Heart Association, Uber, Apple, TEDCO, and Prevention Magazine.
A trailblazer and a role model, Dr. Marvel’s experience in digital innovation that brings high-quality patient care to a new level is inspiring. Dr. Marvel’s presentation provided a solid process to follow for future medical digital innovation strategists:
At CIM we are collaborating across the university to explore how digital technologies can address clinical care issues for patients as they age today and tomorrow, hopefully leading to healthier, longer, and happier lives.

Johns Hopkins Bayview Medical Center (JHBMC) held a special recognition ceremony on January 15th hosted by Vice President for Medical Affairs, Dr. Renee Blanding, in the Grossi Auditorium for those who received the prestigious Clinical Excellence Awards at JHBMC at the end of 2019. In her warm remarks, Dr. Blanding emphasized that this is not about healthcare, the industry; this is about patient care. The event drew high profile guests and speakers: JHBMC President Dr. Rick Bennett; Director of Medicine Dr. Mark Anderson; and Mr. Kevin Sowers, President of the Johns Hopkins Health System and the Executive Vice President of Johns Hopkins Medicine.
Appreciative, kind, and eloquent, Vice Dean and Department of Medicine Chairman Dr. David Hellmann said that he thinks our job at Johns Hopkins with regard to each other is to inspire and treasure; “our tripartite mission depends on it.”

It comes as no surprise that many of the recipients are already CIM Scholars:
Dr. Scott Wright: Physician of the Year, Bayview
CIM Scholar Scott Wright, MD, is the Chief of the Division of General Internal Medicine. He co-developed and runs the Miller-Coulson Academy of Clinical Excellence. Through the academy, Wright developed CLOSLER — for “Closer to Osler” — a social media platform with a mission to inspire health care professionals and trainees to reflect on giving exceptional care to every patient. Modeled largely after Dr. Wright’s work in the Miller-Coulson Academy, the School of Medicine developed a second clinical promotion pathway. Additionally, Dr. Wright revamped his clinical practice to provide “transition care” to patients who need an outpatient follow-up two to three days after hospital discharge. His outpatient practice, in partnership with Johns Hopkins Bayview Medical Center, developed an “ambulatory ICU,” where doctors care for sick patients in the outpatient realm, thus avoiding hospitalization.
Dr. Jon Zenilman: Armstrong Award for Excellence in Quality and Safety, Bayview
Dr. Jonathan Zenilman (aka JZ) is with the Division of Infectious Diseases. He created the Johns Hopkins Bayview Medical Center chapter of the Armstrong Institute for Patient Safety and Quality. JZ strengthened it by developing a program that offers grants for research projects. These projects have helped create a community of faculty members devoted to patient safety and resulted in implementation of programs that are increasing patient safety at Johns Hopkins Bayview. The geriatric surgery program is a prime example of how Dr. Zenilman-sponsored research grants have improved the safety of older patients undergoing abdominal surgery. Dr. Zenilman is a CIM Lavinia Currier Scholar.
Dr. Satish Shanbhag: Best Consulting Physician, Bayview
Dr. Shanbhag is the Clinical Director of Hematology and an Associate Professor of Medicine and Oncology, and he is a CIM Scholar. Dr. Shanbhag has expanded the scope of hematological diseases treated on the campus. A busy clinician with a heavy workload, he maintains high standards of care and provides timely consultative help. He is extremely responsive to all curbside consultations in the outpatient and inpatient settings and has excellent personal communication. Dr. Shanbhag has received multiple faculty teaching excellence awards. Recognized for clinical excellence as a member of the Miller-Coulson Academy of Clinical Excellence, he also received the Samuel Asper Award for Excellence in Internal Medicine, presented by the Maryland chapter of the American College of Physicians.

During the ceremony, Dr. Blanding asserted that JHBMC is already achieving the Johns Hopkins Medicine’s Innovation 2023 Strategic Plan: pushing the boundaries of science and education; working like one organization; supporting the well-being of our people and our communities; improving the quality and affordability of health care; aiming for precision in everything we do; and making Johns Hopkins Medicine easy. Together, WE are making medicine a better public trust. To view the complete list of awardees throughout the Johns Hopkins System, visit: Johns Hopkins Medicine Clinical Awards
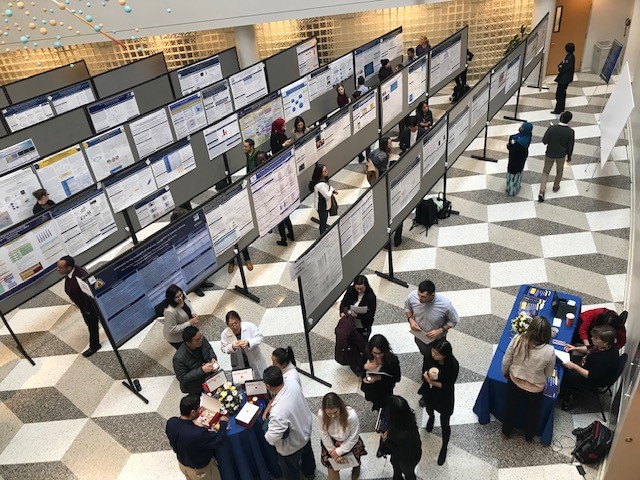
Under the leadership of CIM Lavinia Currier Scholar Dr. Nadia Hansel, who serves as Associate Dean for Research and the Chair of the Johns Hopkins Bayview Scientific Advisory Board, JHBMC happily hosted the Annual Research Symposium on December 6th. This year, Alafouzos CIM Scholar Dr. Kostas Lyketsos had the pleasure of introducing keynote speaker and Nobel prize-winning Dr. David Asch from Penn Medicine, who delivered a highly-informative and quite entertaining lecture on “Health Care Innovation and Behavioral Economics.” The speech was a cornucopia of information about how Behavioral Economics combined with positive psychology can have a significant impact on modifying behavior. Here’s a key take-away message from Dr. Asch, “Once you realize how people are irrational, you are in a better position to help them.”

Also, Dr. Asch encouraged us to get the big picture on behavior modification in the health care industry. Dr. Asch asserted that new and engaging technology in tandem with a keen understanding of human behavior can result in scalable health care change. “Effective nudges” are key. Dr. Asch believes that today we understand human behavior better than we did just a decade ago, that wireless devices make it easier to have high-touch contact with patients, and that financing shifts in the field of medicine motivate providers to connect with people when they are not actually in the presence of their providers. This is the forward-thinking goal of medicine, one with which we can clearly and intentionally motivate ourselves to make it a better public trust by design.
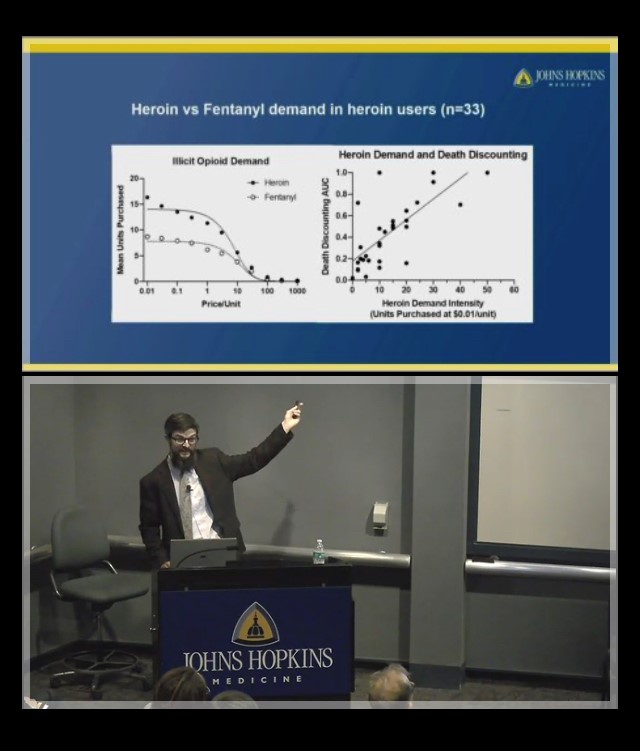
Another featured speaker was Dr. Matthew Johnson, who co-directs the newly formed Johns Hopkins Center for Psychedelic and Consciousness Research, which was recently featured on 60 minutes—you can watch the episode here. His talk on “Behavioral Economics of Drug Use and Related Risk Behavior” complemented Dr. Asch’s lecture to provide a look into how Behavioral Economics plays out in many addiction medicine scenarios.
Overall, symposium attendees took away a greater sense of how people make decisions and/or defer consequences of making poor decisions; consequently, we gained insight into what can motivate a person to make healthy decisions and take strides in the right direction on their path to wellness. The Bayview Research Symposium was a great way to show case our work. More than 240 people flowed through the events all day, including 115 poster presentations, the keynote speech, and our highlighted speaker, as well as an expert panel.
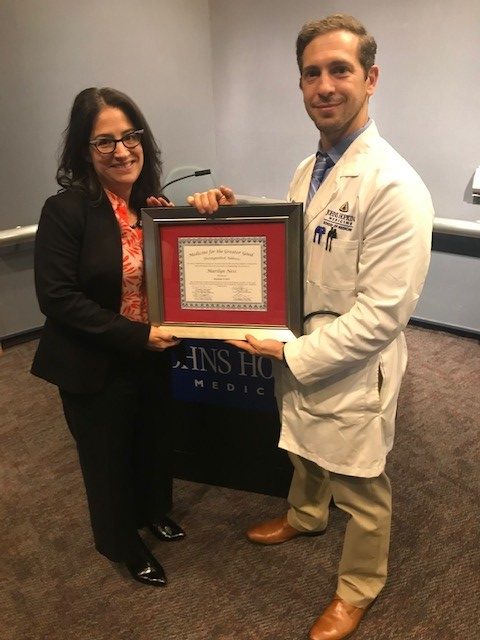
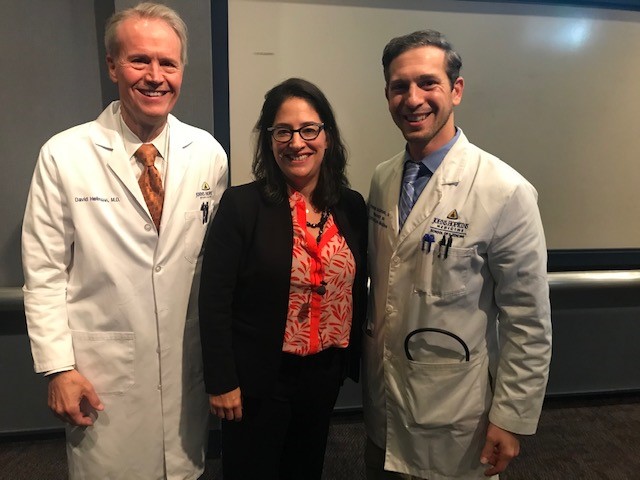
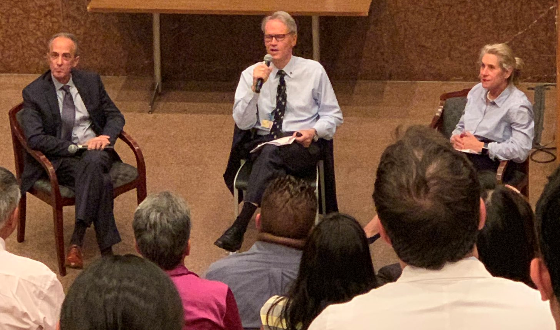
The Center for Innovative Medicine, along with the Center for Medical Humanities & Social Medicine, proudly sponsored Medicine for the Greater Good’s Annual Symposium on Tuesday, November 5th. In its fourth year, it is hard to imagine Bayview without it; it attracts the best creative visionaries working towards making medicine the best public trust it can be. This year’s theme was “Art and Medicine: Partners for Healthier Communities.” The symposium included a spectacular poster session, a fabulous keynote speaker, and a highly engaging panel discussion.
Dr. David Hellmann welcomed a full house in the Grossi Auditorium for the opening of the symposium. He aptly described the goal of MGG to make our world better by training physician citizens to become involved in the community to earn the trust and to work with the community to improve health. MGG co-founder Dr. Panagis Galiatsatos credited the late Baltimore Congressman Elijah Cummings with helping to lay the foundation for MGG’s effective community engagement. Those present remembered him with a moment of silence before welcoming the keynote speaker.
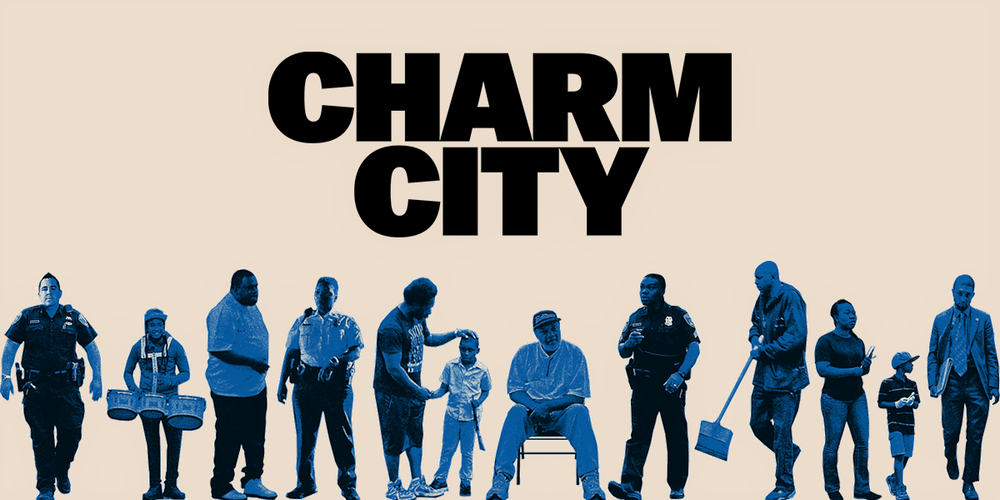
MGG’s keynote speaker, two-time Emmy winning film producer/director Marilyn Ness of Big Mouth Productions spoke about “Building the World of Charm City.” Her film Charm City, a documentary about grassroots, effective community engagement in Baltimore, explores the often acrimonious relationship between the police and “the policed”—who are often striving to improve life in the city. Ness’ spellbinding storytelling is deep healing art–fostering compassion, bridging gaps, and building trust. In the Q&A after her talk, Marilyn Ness said, “you need to show people that they can help.” The documentary premiered at the 2018 Tribeca Film Festival and was shortlisted for the 2019 Academy Award for Best Documentary Feature. Since its release, it has inspired people to help improve their communities. To learn more about Charm City, visit:
After Ness’ speech, the symposium hosted an amazing panel of experts on the serendipity between the arts and humanities and health, healing, and wellness. Asserting that MGG should stand for “Medicine for the Greatest Good,” Dr. Meg Chisholm, Vice Chair for Education for the Johns Hopkins Department of Psychiatry and Behavioral Sciences, moderated a lively discussion with the following fabulous panelists:
A resounding success, the 2019 MGG Symposium was profoundly inspiring, and its theme is absolutely applicable and paramount to healing individuals and communities in Baltimore and beyond. You can view a video recording of Marilyn Ness’ keynote speech here, and the panel discussion here.

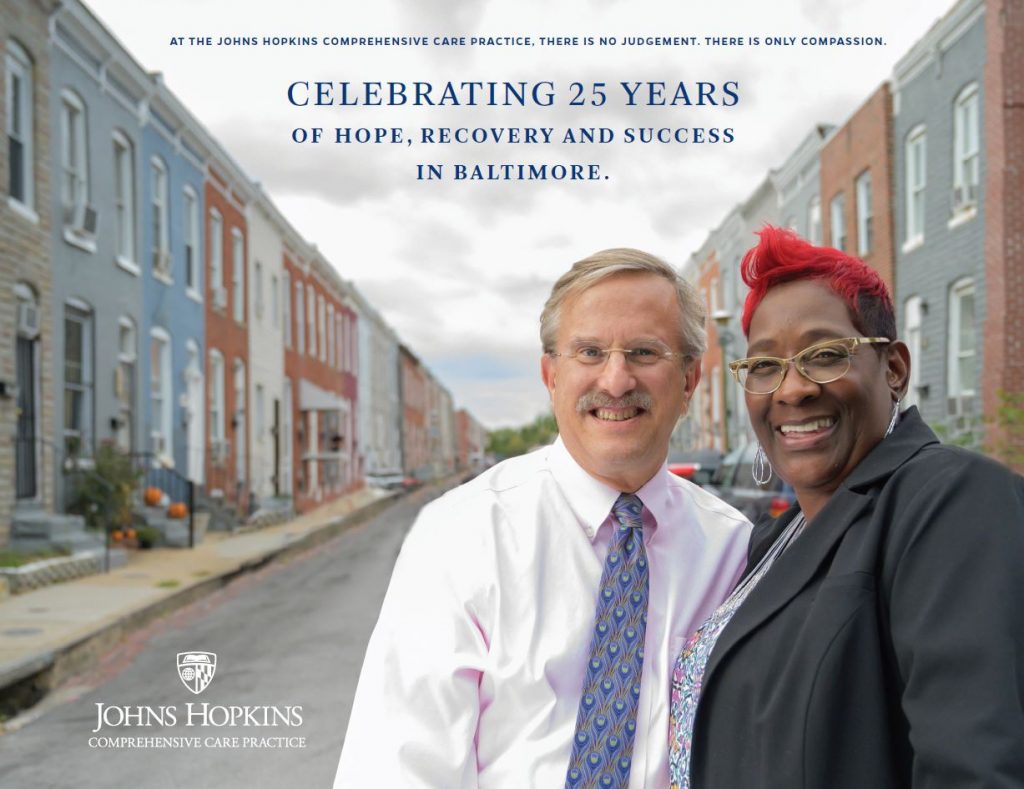
In 2011, Congress designated October as the first National Substance Abuse Prevention Month (NASPM). For the past eight years, NASPM has given the nation a platform to openly discuss and distribute educational materials pertaining to preventing and combating addiction. At Johns Hopkins Bayview, the Comprehensive Care Practice (CCP) team has been in the trenches doing this work every day for a quarter of a century.
Under the leadership of CIM Member Dr. Michael Fingerhood, the CCP was founded in 1994 on four core values:
The CCP is an interdisciplinary and patient-centered primary care team. The team includes experts in caring for patients with HIV, Hepatitis-C, and substance use disorders. They emphasize building trust with each patient; Dr. Fingerhood’s philosophy is that the CCP must try hard to reach every patient with a workable treatment plan that provides hope and health, and he leads by example as he teaches the next generation of physicians to become clinically excellent.
With a joint appointment within the Division of Addiction Medicine within the Department of Medicine at Bayview as well as in the Bloomberg School of Public Health, Dr. Fingerhood knows clinical excellence well, and he is a significant thought leader on treating those struggling with substances with both compassion and good medicine. He was an inaugural member of the Miller Coulson Academy of Clinical Excellence and an early blogger for the Academy. He has devoted his life to a love of primary care and to being a passionate advocate for patients with substance use disorders.
The CCP hosted a gathering to celebrate its silver anniversary on November 1. Here is a video with images from the celebration:
And to commemorate the 25th Anniversary of the CCP’s great work, they will publish a special book, Celebrating 25 Years of Hope, Recovery and Success, that captures images and quotes from key players, including many patient testimonials. Here are a few moving quotes from it.
“CCP is at the heart of true community engagement because it reaches into the depths of community trauma and despair and touches people at the point without blame, shame, anger or despair. CCP reaches into the collective community heart, removes the stigma of substance use disorder and helps to transform one individual at a time.” —Selwyn Ray, director of community relations, Johns Hopkins Health System
“Dr. Fingerhood saved my life, and he taught me that everybody, no matter who they are, what color they are, how much money they have, has the right not just to health care, but to quality health care. And that’s what I try to pass on to my clients.” —Monaye Gethers, substance use counselor and lifelong Baltimore resident
The CCP certainly does put the Care in the CCP. The CIM extends heart-felt appreciation for the life-changing medicine and care the CCP has given for a quarter of a century, and we extend our congratulations upon this special silver anniversary of your accomplishments! Keep up the great work!
On Monday, October 14th, the Center for Innovative Medicine’s International Advisory Board (IAB) met at Johns Hopkins Bayview to have a critical and insightful conversation about the center’s role, influence, and efficacy as we move forward with bold and courageous plans for the future.
IAB members are important to guiding and supporting CIM’s programs and initiatives. With abundant examples, the attendees heard about: the lasting change CIM has had on Hopkins’ culture and policies; the impact of CIM scholars—and the dramatic expansion in the number of scholars during the past 18 months; and the growing movement to launch at Johns Hopkins the human Aging Project, which aims to maximize the years of robust health and to minimize the impact of frailty on individuals, families and society. Throughout the day, IAB members heard from Johns Hopkins all-stars, many of the aforementioned are CIM Scholars or Endowed Professors.
We are grateful to them all for taking the time to speak about their research, programs and clinical excellence during the IAB meeting. We owe a debt of thanks to our IAB members and hope you enjoy this video that we created with our great appreciation!
On August 29, 2019, the CIM held its annual summer retreat at Folly Farm, the home of CIM International Advisory Board Chair Stephanie Cooper Greenberg. Committed to making medicine a better public trust, and building upon the results of last year’s small group breakout sessions, this year’s entire retreat had laser-like focus on tapping into the broad talent at Hopkins to envision and design the world’s finest institute dedicated to providing a long and healthy life—for everyone. The Greenbergs were fabulous hosts, the participants were brilliantly engaged, and the synergistic energy yielded promising results—we are moving together in the right direction.
From the outset of the meeting, CIM Director Dr. David Hellmann underscored Hopkins’ triple stranded DNA–caring, science, and justice—as we design and build an Institute for a Long & Healthy Life at Johns Hopkins. This Institute will be able to address one of the most significant medical challenges in our society—an aging population. Given that the health consequences of aging will dominate every developed country for decades to come, we can think of nothing more important or purposeful than fortifying the future with innovation and the concept of Medicine as a Public Trust.
Throughout the day, Dr. Nadia Hansel was a remarkable retreat leader who kept us focused and guided the day. Geriatrician Dr. Jeremy Walston described what a robust, transformative, and trans-disciplinary institute could look like. Many other physicians, nurses, educators, Hospital presidents and other bright minds came together to contribute how this institute could strengthen Hopkins’ vast potential to grow and build upon it’s already successful, world-class medical disciplines.
At the end of the day, it was a memorable event that harnessed the creative thinking of all the geniuses in the room. There is great synergy to establish an Institute on a Long & Healthy Life at Johns Hopkins. Many thanks to our hosts at Folly Farm for a renewing and invigorating retreat. And many thanks to all the participants who contributed great ideas and helped build momentum and synergy. On behalf of all of us at CIM, we are excited about where this may lead!
Please enjoy the following images and summary comments chronicling the productive day.

Olive the Dalmatian and Stephanie Cooper Greenberg, CIM IAB Chair and retreat host, greet participants Susan Magsamen, Dr. Rick Huganir, and Dr. Jimmy Potash upon arrival.

Drs. Jeanne Clark, Michelle Sharp, Sherita Golden, and Patricia Davidson gather inside and reconnect before the meeting convenes.

Everyone enjoyed Folly Farm’s gracious hospitality and lovely setting for lunch outside on a gorgeous day.

Leaders from across the university synergistically participated in the retreat, generating brilliant ideas.

From left to right: Dr. David Hellmann; Stephanie Cooper Greenberg; Dr. Nadia Hansel; Erwin Greenberg; and Dr. Jeremy Walston.

Mark your calendars now and be sure not to miss MGG’s Symposium on November 5, 2019 from 10 a.m. to 3 p.m. at Bayview.
This year’s MGG Annual Symposium presents “Art & Medicine: Partners for Healthier Communities.” The keynote speaker will be two-time Emmy, Peabody, and Dupont award-winner Marilyn Ness. The most recent film she directed, Charm City, premiered at the 2018 Tribeca Film Festival, was shortlisted for the 2019 Academy Awards, and launched a robust and data-driven pilot impact campaign in Baltimore.
Symposia panelists will also include important thought leaders on the matter of medicine and the humanities—many of whom have strong CIM ties. Here is a small sample of confirmed panelists at this time:
Dr. Galiatsatos, MGG Co-Director, believes “Community engagement is essential for population health strategies to succeed and impact public health. Creative and novel strategies are warranted to achieve the meaningful engagement in the community. Art often times results in humanity displaying its best, reaffirming its identity, and establishing roots for a bright future.”
Details: Tuesday, November 5, 2019, 10 a.m. to 3 p.m., Grossi Auditorium, Asthma & Allergy Building, Johns Hopkins Bayview Medical Campus, 5200 Eastern Avenue, Baltimore, Maryland.
More Info: Contact Dr. Panagis Galiatsatos, E-mail mgg@jhmi.edu or call Tel. 443-303-4866.
This event is sponsored by the Center for Innovative Medicine.
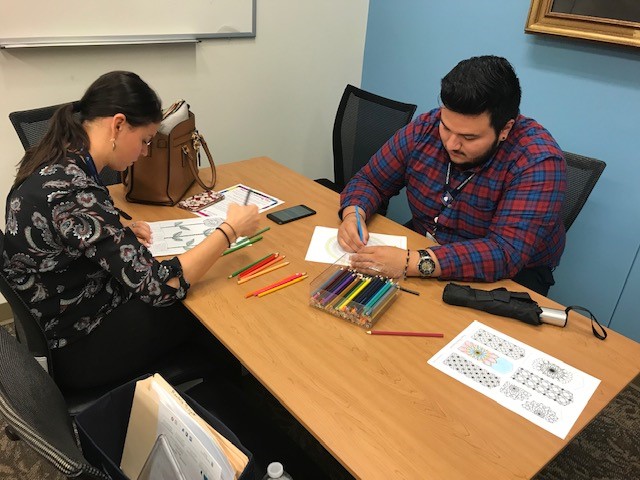
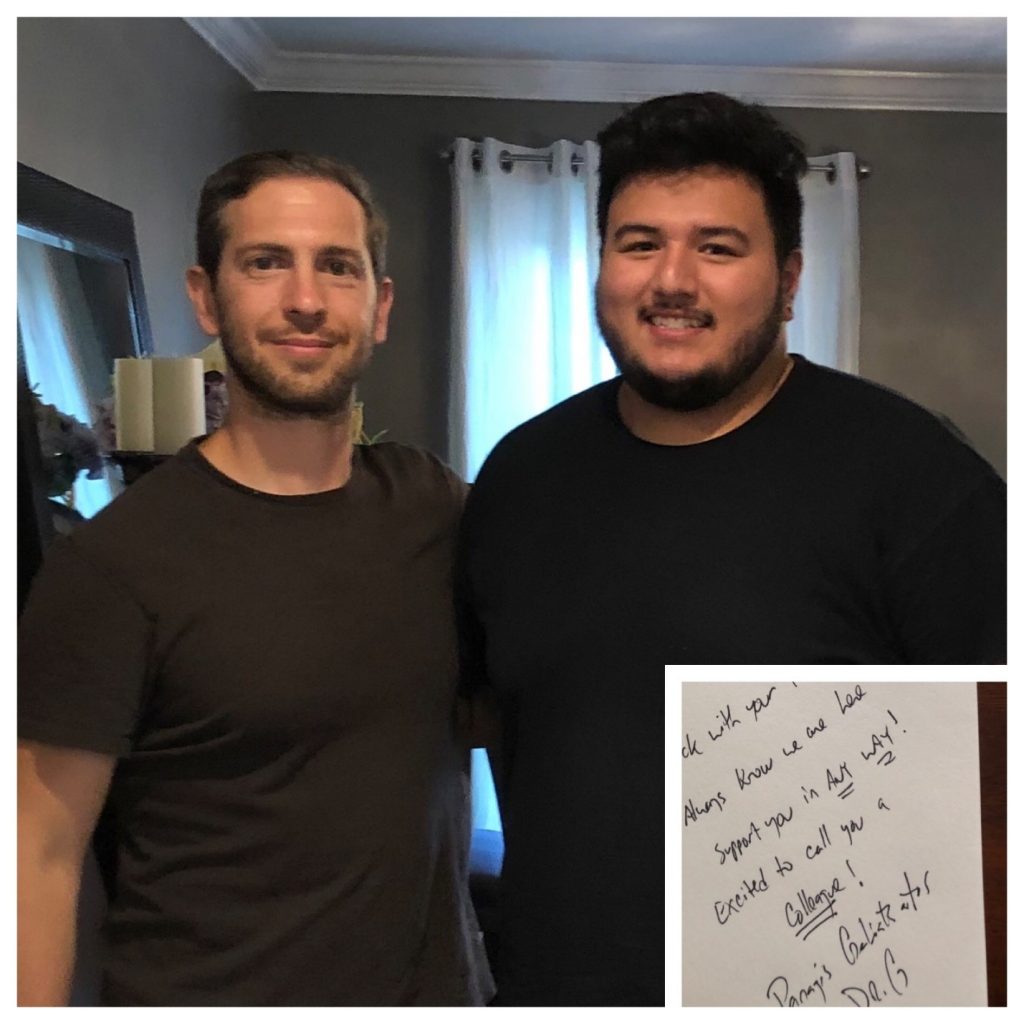
This Summer, CIM and Medicine for the Greater Good (MGG) have been working closely together to support an academic internship with Axel Perez from Berea College in Kentucky. Axel will earn a Bachelor’s in Chemistry with a concentration in Biochemistry and a minor in Biology this December. He intends to go into Osteopathic Medicine, and desires to become actively engaged in the community, which will likely be in a rural area. Consequently, he was inspired to intern with Dr. Panagis Galiatsatos, who takes a great interest in treating each patient as a whole person, and who leads MGG—which is all about community partnerships to address disparities in local health. Axel worked from the CIM office when he wasn’t in the clinic shadowing Panagis or taking advantage of Bayview’s rich programing, such as Grand Rounds, Coloring Towards Mindfulness, and Out of the Lab.
Here’s what Dr. Galiatsatos had to say about Axel:
Our last summer intern, Axel, was drawn to our group for many reasons. One that stood out is his humble beginnings as an immigrant himself, with a strong appreciation for complementing science and medicine with community and compassion. His own personal narrative is clearly a guiding light for him as he weaved into his own professional fabric the essence that defines MGG.
Axel was amazing and at this stage of his career, he already exhibits traits that will make a great physician. Axel took on all tasks presented to him and assisted in strengthening much of MGG’s core objectives: community engagement, equitable healthcare, and social justice. Specifically, his work towards advancing a conversation on family history in susceptible populations has now helped launch “Genetics for the Greater Good,” coming to local schools this Fall and Winter 2019/2020.
Panagis is a superb mentor. He is excited about having an individual intern work MGG because he knows it can be a powerful experience, one that he hopes impacts an intern’s professional identity “in a manner whereby they desire to weave community engagement into the fabric of medicine.”
Axel was an excellent intern. Axel brought with him a wealth of science-based information from his work in the chemistry lab at Berea; combined with his quick recall about biological chemical processes, this experience gave him facility at understanding how diseases, such as Alzheimer’s, progress; at an “Out of the Lab” with Dr. Frank Lin where he discussed his insightful research on this topic, Axel was able to keep pace with the presentation and talk about it on his way back to our office with confidence and ease in layman’s terms. Also, Axel attended a conference on precision medicine, about which he gave a presentation to the Bayview Advisory Board. Below is an excerpt from Axel’s reflection for Berea College about his internship experience with MGG:
Often times after visiting a physician people are left with many unanswered questions, feeling like a burden when asking questions or voicing concerns, and at times being dismissed and put aside by those who we are seeking care from. Events like these are the ones that often times lead to resentment and distrust of members in the medical field, they are also the ones that motivated me to begin my path in medicine.
During my senior year, I was able to join MGG for the summer of 2019, and I was exposed to a completely different culture of medical practice. While working with Medicine for the Greater Good, I was able to change my previous notions and definition of a physician, as a practitioner of medicine, to an understanding and a more refined and personal definition of physician as not only a practitioner of medicine but an advocate for their community’s health culture, who not only prescribes but provides resources and becomes a bridge between healthcare and community members and understands that a patient’s health issues do not disappear when they walk out of the hospital doors and neither do a physician’s duties to their community.
While in Baltimore, I realized that a physician, as well as a community advocate, must in a way be tailored for their community. I quickly realized the importance of having community organizations and physicians who understand and empathize with the community who truly want to help the community and who are consistent in their efforts.
During my internship, I was able to attend and participate in meetings that exposed me to some of the community health issues Baltimore City and see how they impact and amplify socioeconomic and health disparities. These meetings were powerful as they often times revealed the limitations that community organizations and the medical field have all while finding a way to circumvent and, through partnership, overcome these limitations to ultimately elucidate the issues at hand and to strategize a plan to attenuate them.
Axel worked so hard at his internship that we at CIM gave him his favorite car as a parting gift—a Hot Wheels model Tesla! Panagis gave him a copy of his book, Building Healthy Communities through Medical-Religious Partnerships, which will undoubtedly be more useful to Axel than the Hot Wheels Tesla. All in all, anyone who encountered Axel here this summer knows that the road ahead of him is paved with success. We hope he’ll be driving a Tesla around Baltimore one day.

The first weekend in June was Reunion Weekend at Johns Hopkins University, and many School of Medicine alumni were in town on May 31st to attend Medical Grand Rounds at Johns Hopkins Hospital. On that day, the Dean and other high-profile Hopkins leaders packed into Hurd Hall to see Dr. David Hellmann’s presentation on the evolution of CIM entitled, “The Center for Innovative Medicine: Pursuing Medicine as a Public Trust.” On the topic of CIM’s mission, Dr. Hellmann referenced the influence of Kenneth M. Ludmerer’s 1999 Pulitzer Prize-nominated book, Time to Heal: American Medical Education from the Turn of the Century to the Era of Managed Care, which analyzed Johns Hopkins’ historic success, and which led Dr. Hellmann to shape a vision for CIM based on “Hopkins’ triple strand DNA” of caring, science, and justice related to health.
To comment on aspects of CIM’s role as an influential incubator and innovative think tank, Dr. Hellmann invited two guest speakers: acclaimed cardiologist and award-winning teacher, Dr. Roy Ziegelstein, Vice Dean for Education; and Mrs. Stephanie Cooper Greenberg, philanthropist and Chair of the Center for Innovative Medicine’s International Advisory Board. Dr. Ziegelstein described his involvement with CIM to develop a curriculum for the Aliki Initiative, an element of Johns Hopkins Bayview’s Internal Medicine Residency Program which focuses house officers, medical students and faculty to apply the science of medicine to each person. Also, Dr. Ziegelstein credits Dr. Hellmann for finding philanthropy from the Miller and Coulson families to specifically support the clinical care of patients, thus resulting in the establishment of the Miller Coulson Academy of Clinical Excellence, directed by Dr. Scott Wright. The final guest speaker, Mrs. Stephanie Cooper Greenberg, focused her talk on two outstanding examples of ways philanthropists can make relatively small, affordable gifts to make big changes in medicine: CIM Scholars; and Medicine for the Greater Good. CIM Scholarships allow a philanthropist to fund a great idea and partner with physicians at the zenith of problem solving and discovery. Since the initiative began, there have been nearly forty CIM Scholars, and there have been nine new CIM Scholars in the last year alone. Also, Stephanie described how funding efforts through Medicine for the Greater Good appeal to philanthropists because it is a way of impacting the magnitude of vicissitudes in Baltimore through specific, targeted good works.
To watch the a video of the Ground Rounds talk, click here.
In May, the Advisory Board of the Medical Faculty (ABMF) approved an epochal change in the promotion process to include a separate promotional track to recognize and reward clinical excellence that is effective this summer!
Dr. Cindy Rand along with Drs. Scott Wright, David Eisele, and Janice Clements authored and championed the clinical excellence promotions track documents. Before the ABMF voted, Cindy noted how the work of the Miller Coulson Academy of Clinical Excellence, directed by Dr. Scott Wright, paved the way for the creation of the clinical track. Drs. Colleen Christmas, Chris Durso, Steve Kravet, and Scott Wright created the Miller Coulson Academy of Clinical Excellence in 2006.
Having a clinical excellence pathway is a very big deal for Johns Hopkins, its patients, faculty, and students. Clinical excellence is as important as research and education in making Medicine the best Public Trust. You can read more about it here.
This year, Debra Ness, MS, President of the National Partnership for Women & Families presented “Changing the Culture of Health Care – Can We Do It?” for the 16th Annual Miller Lecture at Johns Hopkins Bayview on May 7, 2019.
For nearly 50 years, the National Partnership for Women and Families has advocated to make a better life for women and families by seeking local and national policy changes for equality, justice, economic security including fair pay as well as health care and reproductive rights. Founded in 1971 as the Women’s Legal Defense Fund, the National Partnership for Women & Families is a nonprofit, nonpartisan 501(c)(3) organization based in Washington, D.C., and Debra Ness has diligently moved forward to champion significant policy changes, such as the Family Medical Leave Act, among other things. She believes that achieving equity for all women is key to strong families, healthy communities, and a strong country.
Using data and anecdotal evidence of historical biases in access to quality patient- and family-centered health care, Debra Ness discussed opportunities clinicians may have to affect a culture change in whole-person care, coordination and communication, patient and family support, and timely access as well as meaningful care information. The bottom line to making institutional and industry change happen is that it must start as a result of individual providers committed to making an intentional effort to do it in their practice. You can learn more about Debra Ness’ call to change the culture of healthcare by watching a a recording of the lecture here.
Debra Ness’ presentation at the Miller Lecture was a meaningful contribution to what has become a wonderful tradition. The Miller Lecture was established in appreciation of the Anne G. and G. Thomas Miller family, whose deep and extensive support of Johns Hopkins Medicine has had a significant impact. We were honored to have in the audience Anne G. Miller and her daughter Sarah Miller Coulson. Their generosity, along with Leslie Miller and her husband Richard Worley, helped us establish the Miller Coulson Academy of Clinical Excellence as well as many other exceptional initiatives, including clinical coaching programs and endowed professorships. We are deeply grateful to the Miller family for their support of Hopkins and CIM.
The Johns Hopkins Center for Innovative Medicine (CIM) was proud to present the 11th Annual Miller Coulson Academy Excellence in Patient Care Symposium on Monday, April 15, 2019. Approximately 200 people gathered at the Johns Hopkins Hospital Chevy Chase Bank Auditorium for the Symposium and Miller Coulson Academy of Clinical Excellence (MCACE) induction ceremony.
The Academy received 225 nominations for 67 truly exemplary clinicians, about half of whom submitted extensive portfolios, inclusive of patient testimonials. Of these, only ten clinicians were inducted into the 2019 class, each of whom shared deeply insightful, deeply touching reflections on what shaped their practice and what clinical excellence means to them. And patient testimonials drove home how effectively these physicians practice medicine with care, compassion, and meaningful presence. Here are the members of the MCACE Class of 2019:
Additionally, 23 physicians received the Frank L. Coulson, Jr., Resident Award for Clinical Excellence, and 17 individuals received awards for their superlative roles as a Nurse Practitioner or Physician Assistant.
The 11th Annual MCACE Symposium was a resounding success. The CIM would like to congratulate all of these amazing members of the Johns Hopkins Medicine family, and the CIM would like to thank the Miller Coulson and Worley families for their gracious support to recognize these great clinicians. The CIM recognizes and appreciates the efforts of the many faculty and staff who contributed to the event.
You can watch the recording of the full event here.
Earlier this month, two US Members of Congress from the bipartisan Freshman Working Group on Addiction visited Johns Hopkins Bayview’s Comprehensive Care Practice and Emergency Department with Dr. Mike Fingerhood. Reps. Dave Trone of Maryland’s 6th District and Susan Wild of Pennsylvania’s 7th District sit on the working group of over 40 newly elected lawmakers who are working to promote policies to end the addiction crises. Rep. David Trone, the chair of the working group, shared the following about his commitment to end substance abuse disorder:
“When my 24-year old nephew Ian died of an opioid overdose in 2016, my family experienced the heartbreak of losing a loved one to addiction firsthand. No family should have to wrestle with this kind of grief, yet over 70,000 people died of drug overdoses last year alone. With 192 deaths every day, my colleagues and I are ready to fight back.”
During the visit, the congressmen and their staff met with providers, peer recovery coaches and Health Leads volunteers and took away valuable insights about emergency care medicine and wrap around, ancillary support services for those struggling with treatment. They plan to use this information to introduce legislation making Narcan—the emergency medication to reverse overdoses—is available to all first responders. More footage from the visit can be found here.
Shortly after the Congressional Delegation visited Johns Hopkins Bayview, two regional leaders from the DEA visited and made an expert presentation at our JHBMC Medical Grand Rounds: Ruth A. Carter, Diversion Program Manager from the Diversion Control Division; and Don A. Hibbert, Assistant Special Agent in Charge of the Baltimore District Office and the Drug Enforcement Task Force Strike Force. Their eye-opening presentation focused on the extent of the opioid epidemic in the Baltimore region, and it led to a very interesting Q & A session with JHBMC providers. Sixth on the DEA’s “top 10” list of problem drug areas, Mr. Hibbert believes “we are in the throes of the worst epidemic in 27 years” whereby Fentanyl is driving much of Baltimore’s violent crimes, and it is currently met by the well-known Baltimore Response Model (encompassing coordinated efforts between law enforcement, public health, and community and schools).
The Center for Innovative Medicine is committed to doing our part in fighting the opioid epidemic as we seek to make medicine a better public trust through efforts such good doctoring in addiction medicine (listen to the WYPR podcast mentioned below in the February blog), Medicine for the Greater Good, and “5 in 10”–an effort aimed at increasing life expectancy by five years over the course of a decade in Baltimore City neighborhoods with disproportionately short lifespans.
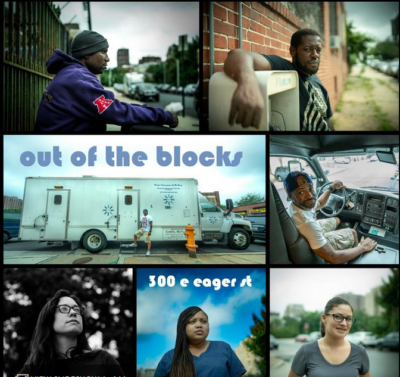 On February 12, WYPR (our local NPR station) aired a segment of “Out of the Blocks” called, “300 E. Eager Street: I’m Fighting for Me.” This series is an immersive listening experience that interviews people to learn about their stories and get to know Baltimore City one block at a time. “I’m Fighting for Me” explores themes of hope, transformation, and wellness in an unlikely place—across the street from the Baltimore City Jail. Yet it is precisely and strategically the right place according to Dr. Megan Buresh, a Johns Hopkins Bayview primary care and addictions medicine specialist; “We know being released from jail is one of the highest risk times for overdose. It’s really hard for people to get into care, and there’s not as much care as we’d like within the system. So we’re here trying to meet people where they are.” Dr. Buresh explains what treatment is (i.e., medication to keep people from craving drugs), and what it is not (i.e., getting high).
On February 12, WYPR (our local NPR station) aired a segment of “Out of the Blocks” called, “300 E. Eager Street: I’m Fighting for Me.” This series is an immersive listening experience that interviews people to learn about their stories and get to know Baltimore City one block at a time. “I’m Fighting for Me” explores themes of hope, transformation, and wellness in an unlikely place—across the street from the Baltimore City Jail. Yet it is precisely and strategically the right place according to Dr. Megan Buresh, a Johns Hopkins Bayview primary care and addictions medicine specialist; “We know being released from jail is one of the highest risk times for overdose. It’s really hard for people to get into care, and there’s not as much care as we’d like within the system. So we’re here trying to meet people where they are.” Dr. Buresh explains what treatment is (i.e., medication to keep people from craving drugs), and what it is not (i.e., getting high).
On an otherwise abandoned city block, a mobile treatment clinic, the “PCARE” van, situates itself across from the jail, where those recently released prisoners battling addiction can walk from the detention center gates directly into the van. In addition to providing treatment, the PCARE van staff serve as a resource for those seeking treatment and recovery and other support.
A PCARE client Travis Lamont Cook, Sr., tells how he became introduced to heroin behind bars. Now 39, he has been in and out of jail about 20 times since he was 17 years old; he says, “Every time I look at that jail back there, it reminds me of every time I’ve been in and out of it and I’m tired of it.” Moreover, people struggle with their past as they look to the future. Brittany Kelly, a PCARE nurse, urges the audience to listen—not just to the broadcast—but also to the real people struggling with addiction issues. Brittany reveals that she is the daughter of an addict, and she has lost several family members to the disease; “People who are addicted have backstories—things that have affected them throughout their lives that you may not have gone through. Before you judge you have to understand their backstory.” In addition to a difficult past, for many people the present is challenging as well as most clients are impacted by homelessness and being surrounded by drugs in their community. Yet, as long as a patient is compliant with their protocol, they deliver treatment—and with it, they deliver hope. To listen to the full piece, please click here.

Our hearts go out to those whose lives were touched by Dr. Nadia Morgan, a doctor in the Division of Rheumatology who was tragically killed in a hit and run crash in December at the young age of 35. Dr. Morgan was a talented and enthusiastic physician-scientist where her robust efforts focused on the impact of race on rheumatic disease. She was an investigator for a multi-center cohort GRASP—the largest study of African Americans living with scleroderma. A promising investigator, a highly respected teacher, a beloved and admired colleague, Nadia was a rising star poised for promotion. Her genuine connection with each person made them feel special. Her sincere caring drove her passion for research. Her gentle, engaging spirit combined with her warm Jamaican friendliness created an absolutely authentic, glowing charismatic persona. Nadia was a truly good doctor committed to making medicine a better trust.
On January 16, 2019, the Johns Hopkins Bayview community honored her life with a fitting memorial service in the atrium of the Allergy & Asthma Center. About 200 people gathered, including Dr. Morgan’s family and friends, to celebrate her life that was cut too short. Remembering Nadia prompted hugs, tears, songs, and laughter. The simple atrium became a sacred space of loving care. Through the heartbreak, the reflections on Nadia revealed a common thread: how impactful her care was to patients, to family, to friends, to colleagues. CIM Director Dr. David Hellmann, who also worked with Nadia in the Division of Rheumatology stated in a moving eulogy, “She had an unusual ability to light up a room…. She was the sun that radiated warmth to anyone lucky enough to enter her world. No wonder our world suddenly felt colder and looked darker on Dec. 15, the night the sun of her bright life was completely eclipsed by a horrific accident.” Dr. Hellmann continued to describe a testament to Dr. Nadia Morgan’s enduring impact a month after her death; Nadia’s office door was adorned with cards replete with heart-felt notes. Several bouquets of fresh flowers respectfully graced the entrance in front of her door. The door still had a sign that Nadia had made about scleroderma awareness that said, “Hope Matters.” Dr. Hellmann asserted that hope and love make us grateful for Nadia’s life.
The Bayview community is grateful to Nadia’s family, Dr. Antony Rosen, and the entire Division of Rheumatology faculty and staff for arranging the service, bringing us together for support to process the painful loss and to remember in joyful appreciation the enduring impact Dr. Nadia Morgan. Let us continue to care for one another, and feel the inspiration of hope that Nadia’s light-filled memory brings. To view a recording of the memorial service, or to contribute to the Dr. Nadia D. Morgan Fund, please click here.